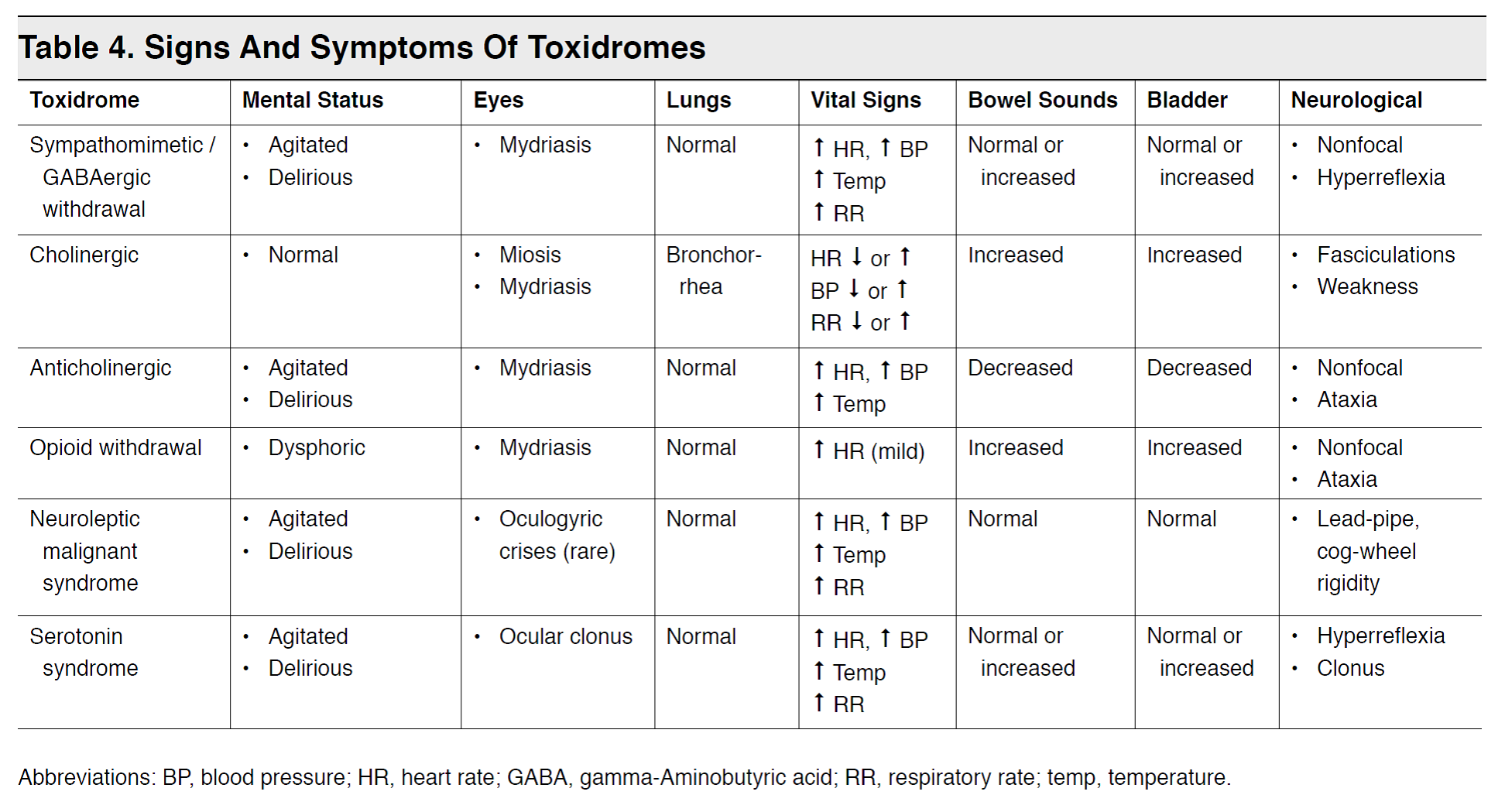
Toxidrome Chart
Toxidrome Chart - Anticholinergic toxidrome, cholinergic toxidrome, opioid toxidrome, sympathomimetic toxidrome. Toxic syndrome or toxidrome is a constellation of toxic effects comprising a set. The major toxidromes most commonly associated with therapeutic use of medications, overdose exposures, substance abuse, and/or poisonings are cholinergic toxidrome, anticholinergic. Review appropriate use of reversal agents including flumazenil and naloxone. Web these toxidromes focus on acute signs and symptoms caused by inhalation and dermal exposures, and each toxidrome is characterized by exposure routes and sources, organs/systems affected, initial signs and symptoms, underlying mode of action, and treatment/antidotes. K2, spice), synthetic cathinones (e.g. ^consider sympatholytic when looking at sedative od or someone who doesn't respond to narcan. Cocaine, amphetamines, ephedrine, thyroid hormone, mdma, pcp, lsd, newer designer drugs such. Pupils 2mm bilaterally, tears running from eyes, hypersalivation chest: (see general approach to drug poisoning in adults.) Web this article reviews the general approach to the poisoned patient, specifically focusing on the utility of the toxidrome. Web a toxidrome is a constellation of findings, either from the physical examination or from ancillary testing, which may result from any given poison. Several organ systems impaired by poisoning. What is toxic syndrome/toxidrome and why is its recognition important? Anticholinergic. What is toxic syndrome/toxidrome and why is its recognition important? Toxic syndrome or toxidrome recognition is important for rapid detection of the suspected cause and helps focus the differential diagnosis to those few chemicals. Soft, nontender, fecal incontinence neuro: Web are you sure you want to sign out? After ingestion, acetylsalicylic acid is converted to salicylic acid. Altered, confused, calm, intermittently vomiting heent: Encephalopathy (from agitation to lethargy), hyperpyrexia, noncardiac pulmonary edema. Pupils 2mm bilaterally, tears running from eyes, hypersalivation chest: Poisonings are commonly encountered in critical care medicine. Patients can be exposed to potential toxins either accidentally (eg, drug interactions or occupational exposures) or intentionally (eg, substance abuse or suicide attempt). Poisonings are commonly encountered in critical care medicine. The patient was admitted to the floor and initiated on heparin anticoagulation therapy. K2, spice), synthetic cathinones (e.g. After ingestion, acetylsalicylic acid is converted to salicylic acid. This is the most important clinical finding. Web timing & amount of ingestions. After ingestion, acetylsalicylic acid is converted to salicylic acid. Recognizing common toxidromes will assist your assessment and treatment of the exposed patients, even when the specific toxin is unknown. Fine rales bilaterally, tachypneic cv: The patient was hospitalized four days ago with severe chest pain and left lower limb swelling, and he was subsequently. Several organ systems impaired by poisoning. Fine rales bilaterally, tachypneic cv: After ingestion, acetylsalicylic acid is converted to salicylic acid. The symptoms of an anticholinergic toxidrome include blurred vision, coma, decreased bowel sounds, delirium, dry skin, fever, flushing, hallucinations, ileus, memory loss, mydriasis (dilated pupils ), myoclonus, psychosis, seizures and urinary retention. Soft, nontender, fecal incontinence neuro: Recognize characteristics of common toxidromes. Web the basic mechanisms, presentation, and management of anticholinergic poisoning are reviewed here. The major toxidromes most commonly associated with therapeutic use of medications, overdose exposures, substance abuse, and/or poisonings are cholinergic toxidrome, anticholinergic. Altered, confused, calm, intermittently vomiting heent: Fine rales bilaterally, tachypneic cv: Web anxiety, cns agitation, seizures, diaphoresis, delusions, psychosis, active bowel sounds, mydriasis that responds to light. After ingestion, acetylsalicylic acid is converted to salicylic acid. Review appropriate use of reversal agents including flumazenil and naloxone. Web this article reviews the general approach to the poisoned patient, specifically focusing on the utility of the toxidrome. It serves to clue the clinician. The patient was admitted to the floor and initiated on heparin anticoagulation therapy. Recognize characteristics of common toxidromes. Common poisoning syndromes to know. Tachycardia, tachypnea, htn, dilated pupils, sweaty, agitation/paranoia; After ingestion, acetylsalicylic acid is converted to salicylic acid. The patient was admitted to the floor and initiated on heparin anticoagulation therapy. Patients can be exposed to potential toxins either accidentally (eg, drug interactions or occupational exposures) or intentionally (eg, substance abuse or suicide attempt). It serves to clue the clinician into the correct diagnosis. Web the basic mechanisms, presentation, and management of anticholinergic poisoning are reviewed here. Web. Review appropriate use of reversal agents including flumazenil and naloxone. Patients can be exposed to potential toxins either accidentally (eg, drug interactions or occupational exposures) or intentionally (eg, substance abuse or suicide attempt). Web these toxidromes focus on acute signs and symptoms caused by inhalation and dermal exposures, and each toxidrome is characterized by exposure routes and sources, organs/systems affected, initial signs and symptoms, underlying mode of action, and treatment/antidotes. Web toxidromes (portmanteau of toxic + syndrome) are a medical syndrome caused by a elevated levels of a substance in the body, and often secondary to a drug overdose or adverse drug reaction. Web are you sure you want to sign out? What is toxic syndrome/toxidrome and why is its recognition important? Fine rales bilaterally, tachypneic cv: Describe initial management of overdose patients. The major toxidromes most commonly associated with therapeutic use of medications, overdose exposures, substance abuse, and/or poisonings are cholinergic toxidrome, anticholinergic. Discussions of specific agents that can cause an anticholinergic toxidrome and the general approach to the poisoned patient are found separately. Toxic syndrome or toxidrome recognition is important for rapid detection of the suspected cause and helps focus the differential diagnosis to those few chemicals. Five commonly encountered toxidromes (toxicology syndromes) are described below along with a summary table of vital sign abnormalities and physical. Web this article reviews the general approach to the poisoned patient, specifically focusing on the utility of the toxidrome. (see general approach to drug poisoning in adults.) This is the most important clinical finding. T 35.2 p 48 bp 100/40 rr 30 gen:
Toxidromes EB Medicine

Toxidromes Compared Anticholinergic, Cholinergic, GrepMed

A toxidrome is a syndrome (set of symptoms) caused GrepMed

Cholinergic Toxidrome Cholinergic, Pharmacology, Medical laboratory

Toxidrome Recognition and Response in ChemicalWeapons Attacks NEJM

CME Common Toxidromes Charlie's ED
Emergency Medicine EducationToxcards Sympathomimetic vs
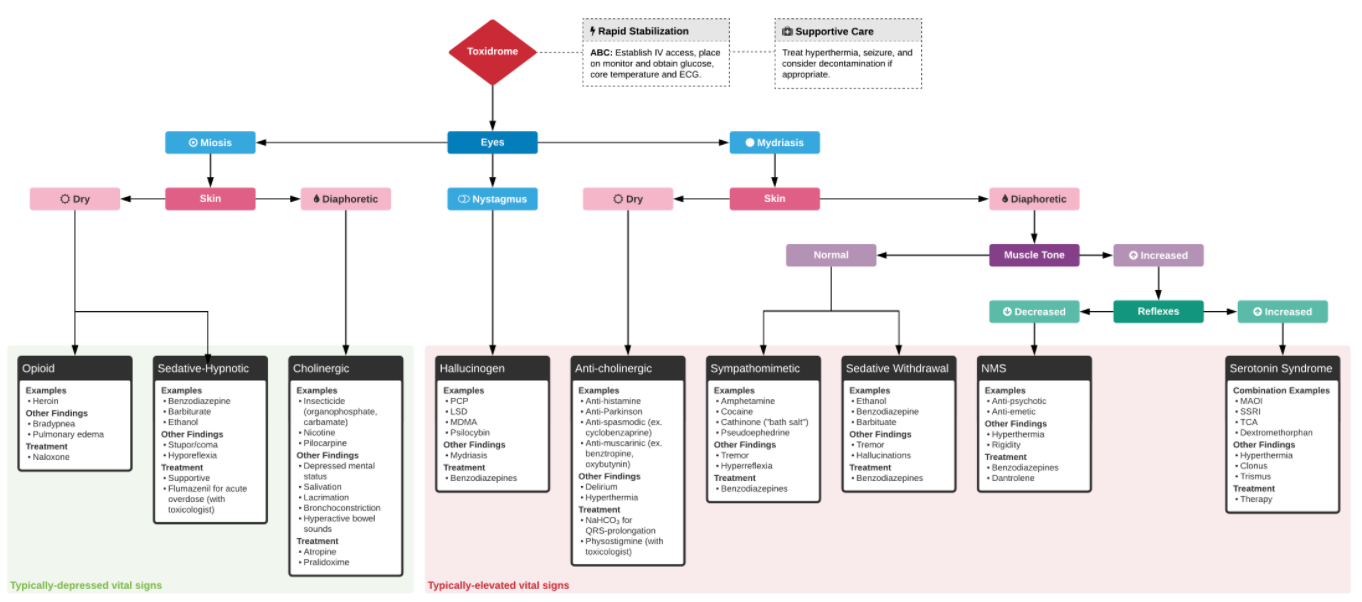
Click here to be taken to a clearer and larger example of the above

Student Paramedics on Tumblr
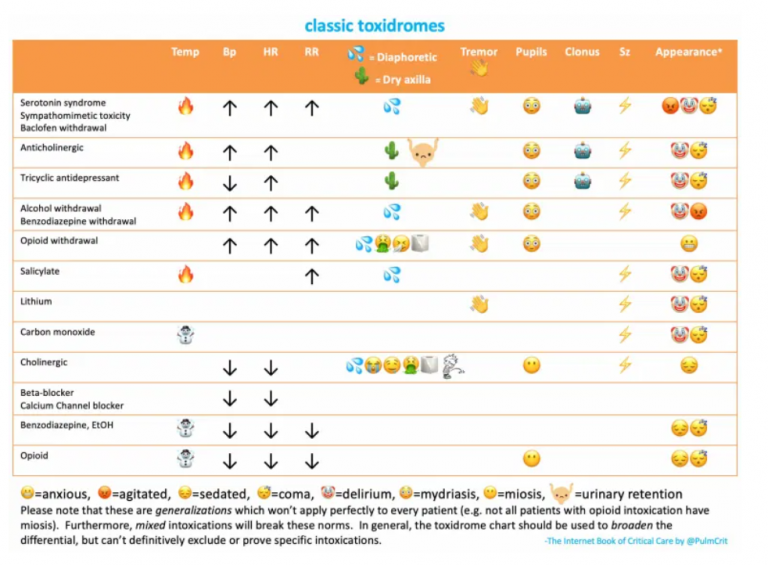
And now, from Dr. Farkas’ Book of Critical Care [link is to
Encephalopathy (From Agitation To Lethargy), Hyperpyrexia, Noncardiac Pulmonary Edema.
Web A Toxidrome Is A Constellation Of Findings, Either From The Physical Examination Or From Ancillary Testing, Which May Result From Any Given Poison.
Common Poisoning Syndromes To Know.
Poisonings Are Commonly Encountered In Critical Care Medicine.
Related Post: